The Intelligent Spinal Biomechanics Research Centre (ISBRC) is a cross-faculty, cross-discipline and cross-institution collaboration dedicated to the enhanced assessment of spinal biomechanics using advanced imaging and data science techniques in the diagnosis of persistent spinal pain and disability.
Little is known about the mechanisms underlying many musculoskeletal spinal disorders, which makes it challenging to develop and apply effective preventive strategies, treatment modalities and rehabilitation plans. Musculoskeletal modelling and simulations represent an attractive approach to non-invasively investigate the relationships between spinal structure and function, however, most of these models are based on generic morphologic properties and few modelling studies incorporate subject-specific properties, specific spinal disorders, and/or measurement of spinal motion in patients.
A number of longstanding collaborations between BU and other research institutes has enabled the advanced study of changes in spinal motion, muscle activation and spinal loading resulting from various spinal disorders including (but not limited to) specific or non-specific back pain, spinal deformities (e.g. scoliosis) and degenerative spinal disorders. The next step is to optimise the measurement of the biomechanics of the living spine using quantitative fluoroscopy (QF) and artificial intelligence (AI) to make biomechanical measurements possible in clinical practice.
Below are examples of our current research activity.

Tracking the bones under the skin: Towards automated spine biomechanics - The MRC AI Spine Dynamics Project (MAID)
Measuring spine dynamics is a complex business, given that the vertebrae are deep in the body and the interactions between them during the simplest of bending tasks constantly change. Yet to detect impairments in spinal function, we need to quickly perform complex calculations from hundreds of X-ray images of vertebrae that are not necessarily either pretty to look at or easy to precisely locate! This is a job for Artificial Intelligence, and with a grant from the Medical Research Council, our team at the ISBRC is now at the start of an exciting new project to develop AI workflows to make vertebral motion analysis in patients with complex spinal conditions both automatic and fast!
Over some 12 years, we collected over 125 standardised sets of QF images of the movement of the lower four vertebrae in the lumbar spine in pain-free healthy controls, standing and lying (passive motion), forward-backward and left-right. This constitutes the largest database of continuous intervertebral motion in existence. It gave us the space to seek out the best measures for making patient-specific comparisons in clinical practice, which we now know includes the evenness of the contributions of each intervertebral level to the motion.
When we examined the motion patterns of vertebral contributions throughout the motion, we found each to be constantly changing, but remarkably distinctive and consistent, constituting the human phenotype for this kind of motion. As intervertebral stability has long been defined as the ability to follow normal patterns of motion, this means that anyone with QF equipment can determine if the stability of each of the lower lumbar segments is normal or not. We also conducted a small sub-study comparing some healthy pain free participants with patients with chronic, nonspecific back pain, which found that patients evidenced significantly less motion at the lowest vertebral level than controls – another apparent biomarker.
The normative database has been published online and is freely available for download when it may be used to allow continuous intervertebral kinematics to drive dynamic models of joint and muscular forces, as well as reference values against which to make patient-specific comparisons in suspected cases of lumbar spine motion disorders.
Intervertebral motion biomarkers for chronic, nonspecific back pain
A number of previous studies have compared spinal motion in people with and without low back pain, measuring how far, and how fast the vertebrae tilt and/or slide. However, these investigations were generally limited by the inability to access detailed, continuous intervertebral motion and to measuring motion at the skin, using methods such as optical motion capture. In more detailed studies using QF and supported by grants from the European Chiropractors Union Research Fund, we also found very little difference, until we started to measure the motion patterns and not just the end ranges.
In a series of studies, we discovered that the overall evenness of the motion patterns was much disrupted in patients compared to controls, even when there was no specific pathology in the spine. We also found a link between non-specific back pain and disc degeneration, which correlated with the unevenness of the motion patterns in the patients with back pain. However, when there was structural disruption as well, such as a slipped vertebra (or spondylolisthesis), the unevenness of the motion between the vertebrae was even greater. However, early disc degeneration, long thought to make the vertebral joints less stable, was found to have no effect on stability at all. The uneven patterns were identified as biomarkers, or measurements that correspond with having back pain. Additionally, when studying their measurement properties, we found that they were stable over a reasonable treatment period (6 weeks) and could be measured reliably by trained operators. Further studies into the motion at individual levels during a bending task found further biomarkers in the contributions of different levels as the motion progressed.
Watch the presentation on “Intervertebral motion biomarkers for chronic, nonspecific back pain" by Professor Alan Breen at the Back2Back Research Meeting at St Anne’s College, Oxford on April 7th 2022:
AI for automatic tracking of fluoroscopic vertebral images
The length of time taken to collect and analyse the images in the Reference Database study is testament to the inefficiency of the image processing methodology used, which requires enough operator interaction to make further diffusion of the technology problematical. Nevertheless, the latest orthopaedic biomechanics textbook contains a chapter written by Dr Alex Breen, a visiting fellow in the ISBRC, and is the first to include fluoroscopy as a joint kinematics measurement device. This makes it even more important to improve the operational efficiency of the technology.
Another good reason to try to optimise QF for joint motion analysis is its difficulty in tracking degraded, distorted or occluded images in the fluoroscopic sequences. This can be problematical for patients with conditions such as obesity, osteoporosis and scoliosis.
The application of Artificial Intelligence (AI) to investigate medical images is growing, for example for the screening of images of the lungs for tumours. However, this kind of application is for recognition and interpretation and not for improved image registration and tracking, for which it is necessary to add a further step. If it is possible to use AI for this, it will constitute a leap forward for Information and Communication Technology research.
Combining FE models based on 3-D MRI with intervertebral motion from quantitative fluoroscopy to assess intervertebral stresses during bending motion
The outcomes of currently practiced care pathways for biomechanical disorders of the spine are usually evaluated through clinical tests, medical imaging or questionnaires, whereas the effects on the functional dynamics of the spine remain largely unknown. Within the past decade, several MSK models of the thoracolumbar spine with different levels of detail about the relationships between spinal structure and function in terms of position/motion and internal biomechanical loading have been presented. However, most of these models are based on generic morphologic properties and few modelling studies incorporate subject-specific properties, specific spinal disorders, and/or measurement of spinal motion in patients.
In collaboration with colleagues at the University of Exeter, we have conducted preliminary studies that combined subject-specific motion information from QF with FE models generated from volumetric MRI scans of the same vertebrae and in the same individual. Results suggested that this was a feasible approach but required greater resolution in the MRI images. As part of the pump-priming exercise of BU’s Institute for Medical Imaging and Visualisation, we are conducting a second feasibility study using BU’s 3T scanner. The purpose is to see if higher resolution will allow faster model development and better geometric measurement for matching the models to the QF images. If it does, we will then consider applying for grants to move this work forward with an AI component, so that dynamic loading assessments can be added to the kinematic ones
 A reference database of intervertebral motion in healthy control participants for making patient-specific comparisons
A reference database of intervertebral motion in healthy control participants for making patient-specific comparisons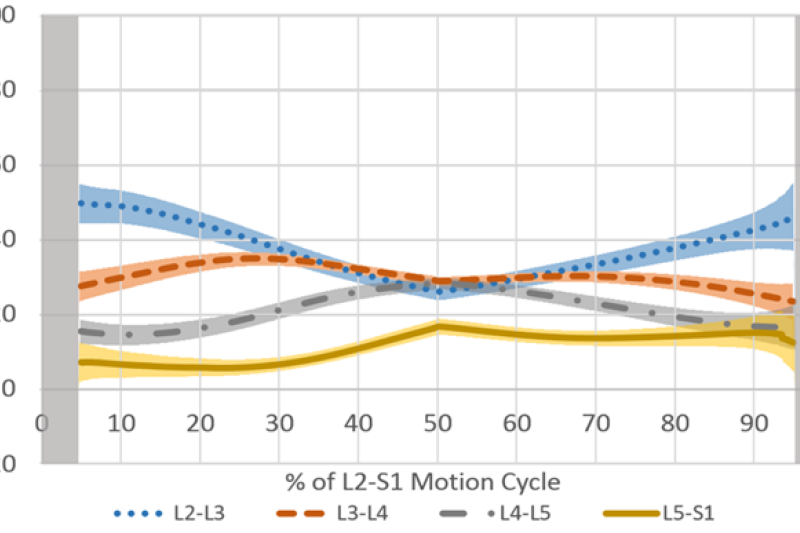 Human intervertebral motion phenotype for lumbar forward bending and return">Human intervertebral motion phenotype for lumbar forward bending and return
Human intervertebral motion phenotype for lumbar forward bending and return">Human intervertebral motion phenotype for lumbar forward bending and return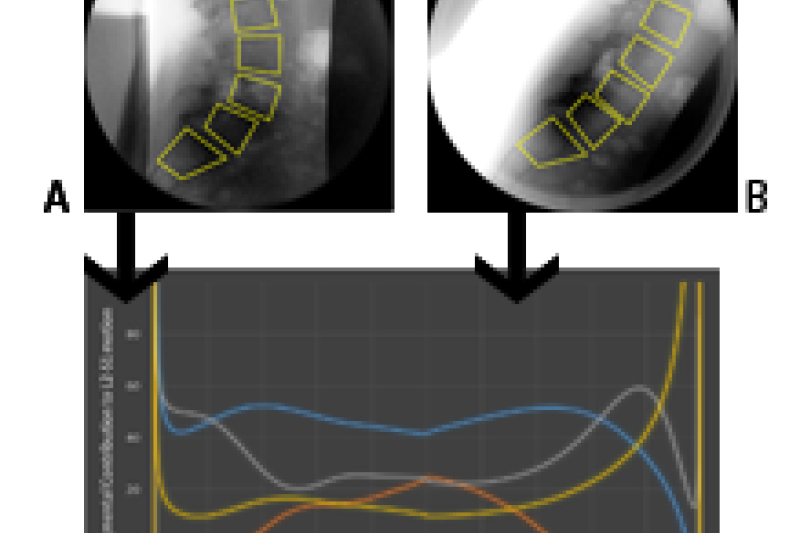 Uneven intervertebral motion sharing in a patient with L4 vertebral slippage (spondylolisthesis) during a forward bending task from start (a.) to full flexion (b)
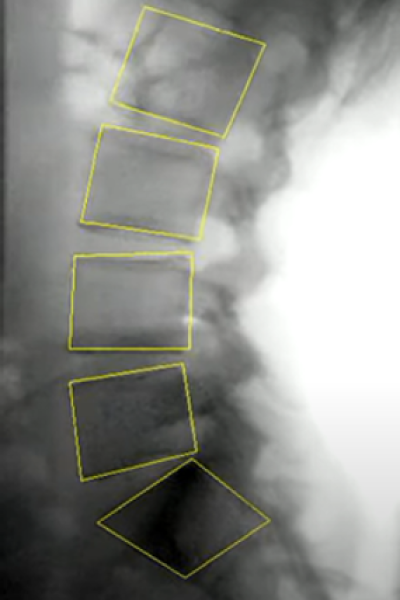
Uneven intervertebral motion sharing in a patient with L4 vertebral slippage (spondylolisthesis) during a forward bending task from start (a.) to full flexion (b) Frame from a fluoroscopic video sequence showing partial occlusion of the L4 vertebrae by bowel gas
Frame from a fluoroscopic video sequence showing partial occlusion of the L4 vertebrae by bowel gas